The Buddy Program
Summary
-
Modeled after the military's "Battle Buddies" program, the Buddy Program at Hennepin Healthcare was created in response to the stress brought on by the COVID-19 pandemic on clinicians
-
The Buddy Program will create a wellness structure based on peer support where providers are paired as “buddies” who check in on each other regularly to provide support during the pandemic at Hennepin Healthcare System (HHS)
-
Oversight and support is provided by department Wellness Champions
-
Additional support is provided by a team of mental health professionals or the Office of Professional Worklife (OPW)
Program Description
The Buddy Program is a peer support program for all clinicians (physicians and advanced practice providers) and is part of a larger effort called the Mental Health Protection Program at Hennepin Healthcare System (HHS).
Modeled after the military’s “Battle Buddies” program and a similar program underway at the University of Minnesota, this evidence-based program will create a wellness structure at HHS where providers are paired as “buddies” who check in on each other regularly to serve as sounding boards, ensure personal stability, and provide each other with support throughout this pandemic. The “buddies” will have the opportunity to check in about stress levels, connect and share concerns or successes with someone who is familiar with what they are facing, and can offer support and community at a time of high demand.
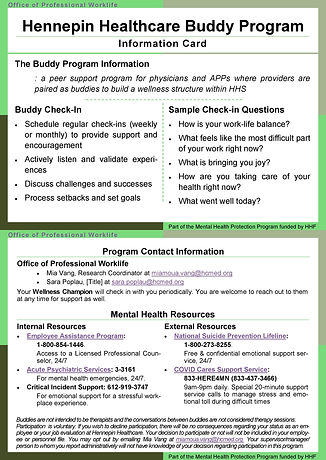
Informational cards which have check-in instructions, sample check-in questions, and contact information for the program & for mental health resources are provided. Departmental level oversight and support is provided by department Wellness Champions. They oversee the provider pairs by checking in periodically, are available to provide additional assistance and address concerns, and can direct providers to a team of mental health professionals or the Office of Professional Worklife (OPW) for further assistance. The program is financially supported by the Hennepin Healthcare Foundation.
Background
The COVID-19 pandemic is taking a tragic toll on patients and a visible toll on clinicians. Front line clinicians are stressed, exhausted, fatigued and scared. Rapid changes in protocols, massive email volume overload, fear of contracting the illness or bringing it home to loved ones, and the emotional impact of watching patients die with little we can do to help them, all conspire to attack any sense of well-being that clinicians might have, and leave them feeling drained, worried, helpless and guilty. Clinicians who are working behind the front line are also facing stressors including concern they are not doing their part, fear of not meeting productivity goals, and frustration at trying to provide care over the phone, at the same time as many are caring for children who are not in school.
Clinicians were already facing stress and burnout before the pandemic. Research by our team (Linzer, JGIM. 2016) and others (Shanafelt, Mayo Clin Proc. 2017) has shown prevalence rates of burnout ranging from 10-50%, with key predictors being time pressure, chaotic workplaces, lack of control, and adverse organizational cultures (such as lack of values alignment between clinicians and leaders, emphasizing productivity over quality, lack of cohesion, and lack of trust in the organization). Our studies have also determined there are interventions that reduce burnout, including workflow redesign and improving communication (Linzer, JGIM. 2015). Dyrbye showed that reducing burnout markedly reduced the risk of suicidal ideation in medical students (Annals of IM, 2008).
The Hennepin Healthcare System’s (HHS) Office of Professional Worklife (OPW) partnered with the American Medical Association to create a “Coping with COVID” brief survey to gather data from healthcare workers across the country and at HHS. Preliminary survey data shows that clinicians are facing stress both at work and home such as fear of transmitting the virus to family and others in the community, feeling like they are failing as clinicians, not having time for breaks or to eat, and feeling drained and unrested. Our team believes that a program aimed at improving clinician mental health and reducing burnout can improve morale while lowering depression and suicide risk, and hopefully prevent PTSD.
Progress
The Buddy Program trial is rolling out in June 2020. Early steps are focusing on connecting with department leadership and gaining administrative buy-in. The decision was made to make the program opt out instead of opt in, so every provider would have someone to watch out for them. Buddy pairs are based on provider type (physician or Advanced Practice Provider) and FTE level within their hospital department.
Each department member is informed of the program via email communication which explains the program purpose and provides the information card, program contact names & emails, and a list of all the buddy pairs for the department.
Lesson Learned
Having a provider wellness structure already in effect was a great help. The Provider Wellness Committee (PWC) was supportive and its members are the departmental Wellness Champions who offer assistance to the buddy pairs. They were also able to provide departmental insights, advice and assistance in creating the pairs. If this structure does not exist in your work place, it can be created by seeking out department leaders (formal or informal) who have an interest in or support wellness work.
We hope to share more about the work and our progress as we implement the program at HHS.